Carver College of Medicine receives $3.7 million to study coronavirus transmission in emergency-healthcare workers
The CDC awarded the UI and UCLA a joint grant for research examining the level of risk emergency health care workers are at for contracting the novel coronavirus.
The Roy J. & Lucille A. Carver College of Medicine is seen on Monday, November 18, 2019.
May 6, 2020
The Centers for Disease Control and Prevention awarded the University of Iowa Carver College of Medicine a joint $3.7 million grant to study how to reduce emergency health care workers’ risk of contracting COVID-19 while treating positive patients.
The study, conducted in partnership with the University of California, Los Angeles David Geffen School of Medicine, will be conducted over a 12-week period and involve 1,600 emergency department personnel from 20 different academic health care institutions across the U.S. The study is called the COVID-19 Evaluation of Risk for Emergency Departments, or COVERED, project.
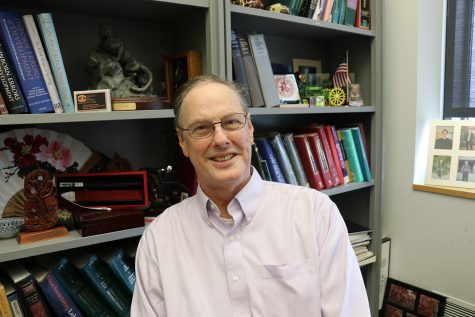
Nicholas Mohr, co-principal investigator of the study and UI clinical associate professor of emergency medicine, anesthesia critical care, and epidemiology, said the CDC showed a lot of early interest in funding the project.
“Over a very short period of time, we wrote a study proposal and the CDC was very enthusiastic about this because this is really one of the most important questions for how we can continue to provide care for patients who have COVID-19,” Mohr said.
Mohr added that this project is a collaboration between two national research networks, EMERGEncy IDNET and the National Emergency Airway Registry. The collaboration between these two networks and other academic medical centers made it possible to roll out a large, multi-center research study so quickly, he said.
“Working around the clock and identifying a very good group of people has allowed us to get the project up and running very quickly,” said David Talan, professor emeritus of emergency medicine and infectious diseases at UCLA and co-principal investigator of the COVERED study. “We put together a very good team of people and we all have worked very hard.”
Talan said that the researchers requested the $3.7 million-dollar grant based upon their own estimates of the necessary funding to complete the study.
RELATED: Carver College of Medicine Hawkeyes provide services for health care workers
“There are 20 sites, and each site has study personnel that are necessary to set up the study and direct it,” Talan said. “There is money for laboratory testing, participants’ time, blood testing, personnel to set up a database system to record the results and keep track of them, so those are some of the main things that go into it.”
Research unrelated to the novel coronavirus at the UI was put on pause in April in an effort to prevent further spread of the virus, as previously reported by The Daily Iowan. While this could pose funding concerns for research at the UI, Mohr said the work itself is more important than the money involved.
“This question is really important for us to figure out as a health system how we can keep emergency departments open and keep health care workers on the job,” Mohr said. “The grant from the CDC really enables that question to be answered in a very rigorous way, and when a grant comes in, that allows us to do a body of work that previously would not have been able to be done.”
According to the UI Health Care website, the project studies four different groups of emergency health care workers with varying interaction among COVID-19 patients, through the use of questionnaires, blood tests, and self-collected nasal swabs. Emergency physicians likely to be performing endotracheal intubation are of major interest, because they are thought to be at the highest risk of contracting the virus.
“Patients going into respiratory failure need endotracheal intubation and mechanical ventilation to stay alive, and what happens during that procedure is that the virus is aerosolized into the air,” said Brett Faine, UI clinical assistant professor of pharmacy practice and science and emergency medicine. “[Physicians] are standing over the patient doing that procedure roughly a foot or two from their face, which is why the providers doing that procedure are at the highest risk.”
Talan said that the researchers hope to draw some conclusions from the COVERED study by the fall.
“We are in a historic moment in terms of mankind and medicine,” Talan said. “We have an obligation to protect not only the people who provide us care but also the people in our communities who rely upon them.”