UI professors expand palliative care education to colleges outside of pharmacy
Professors in the University of Iowa’s College of Pharmacy hope to allow access to their palliative care electives to students in other disciplines.
February 21, 2022
Few people associate health care with spiritual and psychological treatment, according to Delayne Glassgow, a graduate student at the University of Iowa College of Pharmacy.
Palliative care at the UI may change this.
UI College of Pharmacy professors plan to open palliative care courses to other UI professional colleges, including the College of Nursing and the College of Social Work, hoping to form well-rounded emotionally intelligent students.
Palliative care workers treat patients with serious illnesses and do not prioritize the physical or chemical over the psychosocial, psychological, or spiritual.
“A lot of what we’re doing right now in health care is treating the disease and not the person,” Glassgow said. “I want to prioritize the needs of the patient and not their prognosis, not their disease, and it’s kind of a next step for actually caring for patients.”
The UI College of Pharmacy Palliative Care Certificate has been around since 2017, when UI alum and chairman of OnePoint Patient Care James Otterbeck donated $1.5 million to the UI to fund the program.
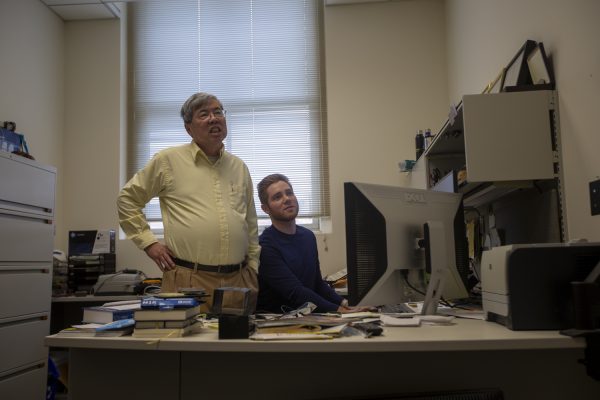
Kashelle Lockman, clinical assistant professor of pharmacy practice and science at the UI’s College of Pharmacy, said extending courses to other colleges would allow students to learn side by side with those of different disciplines, just as palliative care practitioners do in hospitals.
“Our patients really benefit from having that interprofessional approach to patient care and from us working with each other closely and collaboratively,” Lockman said. “It really takes a village, if you will, when you’re caring for someone with a serious illness to help them live the best days that they can live every day.”
Michelle Schmidt, UI College of Pharmacy clinical assistant professor of pharmacy practice and science, said the experiential aspect of the Palliative Care Certificate is most prevalent in an outpatient clinic.
She said the College of Pharmacy also offers Advanced Pharmacy Practice Experiences in palliative care within inpatient and outpatient care settings, as well as at two hospice pharmacy benefit manager rotation sites. A long-term goal is to expand palliative care rotation opportunities, she said.
She said, in addition to adding courses to the curriculum, she hopes to create a more local option for the experiential rotation that students undertake.
“The number of patients that have serious illness in the U.S. is considerable, and so palliative helps provide patients with a framework for navigating a lot of the difficult conversations that occur as they navigate their serious illness,” Schmidt said.
Like hospice practitioners, another branch of palliative workers who focus care on the terminally ill, palliative care practitioners come from a variety of professional backgrounds, including pharmacy, chaplaincy, music therapy, nursing, social work, medicine, and others.
Lockman said the palliative care team went from having a single pharmacist in 2015 to having four this year.
While the College of Pharmacy has its own palliative care electives in addition to the certificate, exclusive to pharmacy students, she said, the College of Nursing and the College of Social Work have some of their own palliative courses.
“We just haven’t had the bandwidth to open it up to more students yet, so having more faculty in palliative care will help us get there,” Lockman said. “Collaborating with the other colleges and schools will help us get there too.”
Every year, Lockman said, about 10 percent of the pharmacy class enrolls in the certificate, which is 17 credit hours added to an already intense curriculum.
“We also integrate some palliative care content into our required courses, so all the pharmacy school graduates will sit in class for at least fifty hours, working on palliative care topics and learning palliative care topics,” Lockman said. “Thirty-two of those hours have been pain management and then eighteen hours have been non-pain palliative-care-related topics.”
Lockman also said the third 2021 graduating class that took part in the certificate was larger than the first, comprising thirteen students compared to 2019’s eight students.
“So, it’s been nice to see students are interested in this topic, and we’ve gotten feedback,” Lockman said. “We did a little survey of the students and the students who graduated with the certificate felt like they really developed emotional intelligence through the courses, and they also developed skills to navigate personal loss in their own lives.”
Schmidt said many colleges of pharmacy across the country palliative care education are limited and the college may not have palliative care trained pharmacist as part of their faculty.
“Most universities, if they have any, it’s usually just one,” she said. “And that’s true in most specialties, there’s usually one at most two faculty within each specialty.”
According to the Center to Advance Palliative Care, one-third of U.S. hospitals have no palliative care offerings.
Of the seventeen credit hours necessary to complete the certificate, Lockman said any student in the College of Pharmacy can take up to sixteen hours. She said that 220 students have taken at least one palliative care course.
“So that’s a pretty big impact because we didn’t have that many hours in our curriculum, it was a few hours here and there and so now we have a lot more content in our required courses,” Lockman said.
Correction: The DI reported that the palliative care team went from having a single pharmacist in 2017 to having four this year. It was in 2015, not 2017. The DI also falsely reported that team management is part of the certificate. It is pain management. The DI regrets the error.