Opinion | Why it is vital to think about timing for Medicaid
Millions of Americans are at risk for losing Medicaid, it is vital to take them into account without a rush of process.
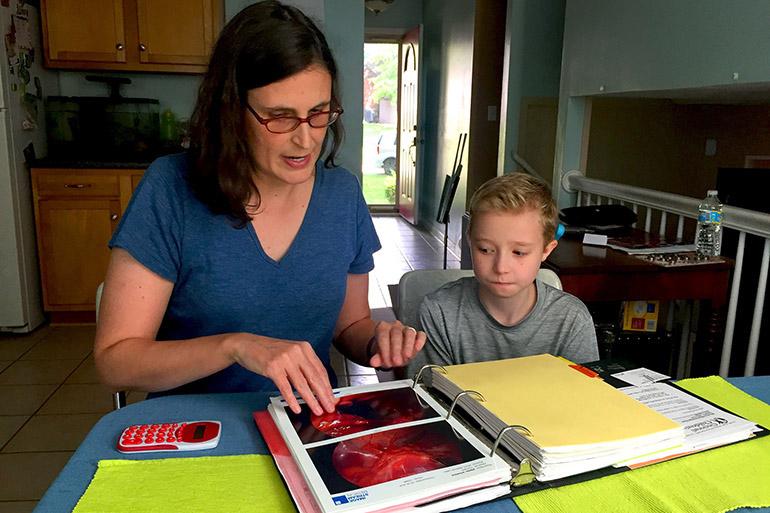
Ann Pipes and her 11-year-old son, Winslow, go over Winslow's medical records and aid his public school is required to give him through the Americans with Disabilities Act. Winslow has a craniofacial disorder and severe hearing loss he was born with. Winslow depends on Medicaid coverage for his care, which has included 14 surgeries starting when he was an infant. (Lisa Gillespie/Kaiser Health News/TNS)
April 11, 2023
Millions of Americans are at risk of losing Medicaid.
Following COVID-19, state officials are beginning to determine which individuals are no longer eligible for health care coverage under Medicaid.
The U.S. Department of Health and Human Services announced that 7 million Americans will lose Medicaid. Reasons for this loss of coverage involve incomplete or lost paperwork and the basis of one’s income, which means people who earn too much will be cut from the program.
This rushed process is concerning. Americans should be given the time they need to ensure that they have an alternate well-fitted program or a safety net, at the very least.
Depending on the individual, loss of coverage can happen by not being able to provide the materials that are needed to verify one’s income or residency. However, these can often get lost in the mail or take a long time to retrieve and receive.
Gov. Kim Reynolds said that it is time to move ahead, and it’s time to move forward because the pandemic is in the past. She concluded by saying that the Public Health Emergency is negatively impacting the states and that there are an overwhelming number of individuals under the cover of Medicaid.
For Iowa’s disenrollment process, the state determines whether or not an individual will remain under coverage. If the individual is determined to no longer qualify for Medicaid or has not given proof to officials of their coverage in a timely manner, they will be cut off from the program.
Iowa began its disenrollment process April 1. First cut offs are expected in May.
As of December 2022, 874,481 Iowans are on Medicaid, according to the Iowa Department of Health and Human Services. Around 136,000 individuals are expected to be cut off from Medicaid in the disenrollment process.
Millions of people are on the verge of losing Medicaid, and state officials do not seem to be fully aware of just how many individuals will be affected in this short amount of time. Millions could be left stranded with no means of health care coverage or support.
A rush in the process is unfair to those that need Medicaid insurance. Instead of attempting to rapidly cut off individuals from the program, state officials should keep in mind that many individuals often need extra time or attention to gather their needed materials for eligibility.
It is important to note that many people are unable to efficiently switch to other health care programs, thus leading them to have no coverage or support if they were to be disenrolled from Medicaid.
States should keep in mind that to meet the needs of their people, they will need to take their time in doing so. Everyone has their own set of possible problems for meeting eligibility deadlines, so it would do states good to take their matters into account with patience.
Millions of Americans are unsure of where they stand in terms of health care coverage, and this can often be a stressful moment in time. They deserve a safe landing and a hand they can reach out to.
Columns reflect the opinions of the authors and are not necessarily those of the Editorial Board, The Daily Iowan, or other organizations in which the author may be involved.