Researchers use chatbots to deliver psychotherapy to help decrease opioid use
Researchers at University of Iowa Hospitals and Clinics and University of Pennsylvania Medicine developed artificial intelligence software that helps patients who are experiencing pain after trauma surgery understand how to cope, rather than patients turning to opioid pain medication.
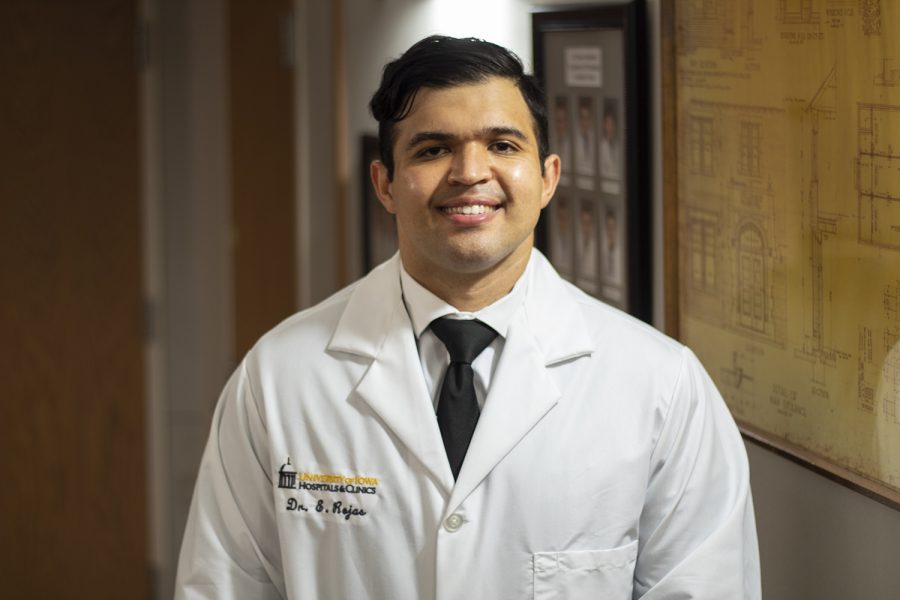
Pictured on Aug. 31, 2020 is Dr. Edward Rojas inside the Orthopedics and Rehabilitation Center at the University of Iowa. UIHC is carrying out research on how chatbots can minimize opioid usage for patients after surgeries.
September 3, 2020
Researchers at the University of Iowa and University of Pennsylvania are using chatbots, an artificial intelligence software, to deliver psychotherapy to patients to cut down their opioid use after surgeries.
Chris Anthony, the associate director of the Penn Hip Preservation Center at Penn Medicine, collaborated with UI Orthopedics Resident Edward Rojas to study how to address the concern for patients who become dependent on opioids after undergoing trauma surgery.
Anthony said researchers wanted to use technology to reduce the need for opioids and improve patient care.
“Opioid utilization is a really big deal in our country right now,” Anthony said. “We know that when patients use opioids they can become addicted. Being able to use less pain medication is a really big deal in terms of lowering the chances of becoming addicted to medication over a longer term.”
Anthony said he created the chatbot software over a decade ago when he was a UI medical student. He decided to combine his software with psychotherapy, using the help of UI Clinical Health Psychologist Valerie Keffala, he said.
The chatbots are programmed to send text messages to patients twice a day, Anthony said.
According to the study, 76 orthopedic patients at UI Hospitals and Clinics were randomly divided into two groups. Each group was prescribed opioid medication, but one group received two text messages per day over a two-week period from a computer that used artificial intelligence software, Rojas said.
The researchers used acceptance and commitment therapy, which helps patients move through their difficult feelings, rather than stop them, Keffala said. Keffala developed statements to normalize the patient’s experiences.
The chatbots used affirmation to validate a patient’s pain, hoping to discourage the use of opioids, Anthony said.
“If you had to bring it down to one word I would say affirmation,” he said. “The chatbot affirmed patients where they were at to encourage them that the current pain they were feeling after surgery is something that is relatively normal.”
Using psychotherapy, doctors can help patients self-regulate and work to prescribe them medication based on their individual needs, Rojas said.
“I think it’s essential that we work on being better stewards of these types of medications,” he said. “They can cause people harm if we do not make very thoughtful decisions regarding how we treat patient pain and the expectations we set for patients following surgery.”
According to the study, the patients who didn’t receive messages took 41 opioid tablets, while the group that did took 26 tablets.
This 37 percent difference is an important indicator of how effective psychotherapy can be, Anthony said.
“People often don’t have exposure to psychological skills that can help them move through that experience of pain very effectively,” Keffala said. “We wanted to give them psychological skills that can help reduce some of that unnecessary suffering.”
The outcome of the research makes the doctors hopeful that patients will be able to rely less on opioid medications in the future, Anthony said.
Rojas said this can significantly improve patient care, especially for those who undergo traumatic injuries.
“This research helps us see that patients — by changing the way they’re thinking and by the way they respond to their pain — can reduce their usage of opioid pain medication after surgery without compromising that pain relief,” Keffala said. “This gives us hope that we can do interventions that are non-pharmacological and bring patients the relief they’re needing.”