Nurse liaisons provide human connection, technology support to patients
Due to visitor restrictions, University of Iowa Hospitals and Clinics and Mercy Hospital nurse liaisons have become the primary human connection for patients and their families.
May 12, 2020
As hospital patients are cut off from visitors, Iowa City nurses have become the sole connection between patients and their loved ones, using human and technological interaction to bring families together amid the COVID-19 pandemic.
Nurses at University of Iowa Hospitals and Clinics and Mercy Hospital in Iowa City place phone calls to family members of patients to provide them with medical updates and use donated tablets to allow face-to-face interaction between patients and their loved ones.
UIHC said in a statement April 14 that it would place restrictions on patient visitors, regardless if the patient’s situation was COVID-19 related or not. UIHC suspended nearly all visitors for adult patients and limited visitors for children to one immediate family member.
UIHC implemented a nurse-liaison program to provide each patient’s family with a nurse as their primary contact. Continuum of Care Management Director Peggy O’Neill, a coordinator of the UIHC nurse-liaison program, said the idea came from a Hospital Incident Command System meeting, which discussed different scenarios in response to the novel-coronavirus pandemic.
“One of our nurses said she made a phone call to a daughter, telling her [that] her mother was on the floor and doing well,” O’Neill said. “That daughter was ecstatic, that someone could tell her that they had seen her mother — had laid eyes on her — and that she was doing OK.”
Another nurse showed a woman how her husband was walking in the hallway after undergoing therapy, she said, and that it was a relief to her to know that the therapy was continuing despite the virus. O’Neill said this virtual communication would be impossible without the accessibility of technology.
“We would not be able to connect as well as we do,” she said. “It’s helpful for [all kinds of] patients. Some patients are able do a FaceTime call with their own families. Those on a ventilator and cannot talk, use Zoom. [The families] know they cannot talk, but they can see them, and that’s important.”
Clinical Service Specialist Jolyn Morgan, a nurse liaison, said the nurses speak to a chosen point of contact, providing them with daily updates on the patient’s condition.
Morgan said the nurse-liaison response increases not only the safety of UIHC employees and patients but reassures families who cannot be there in-person to see their patient’s progress.
“If you know that you are going to get a call every day, that’s more [reassuring] than sitting and wondering,” Morgan said. “It’s a relief for families to know that they will routinely receive an update, and we have a consistent nurse liaison to build a relationship between themselves and the family.”
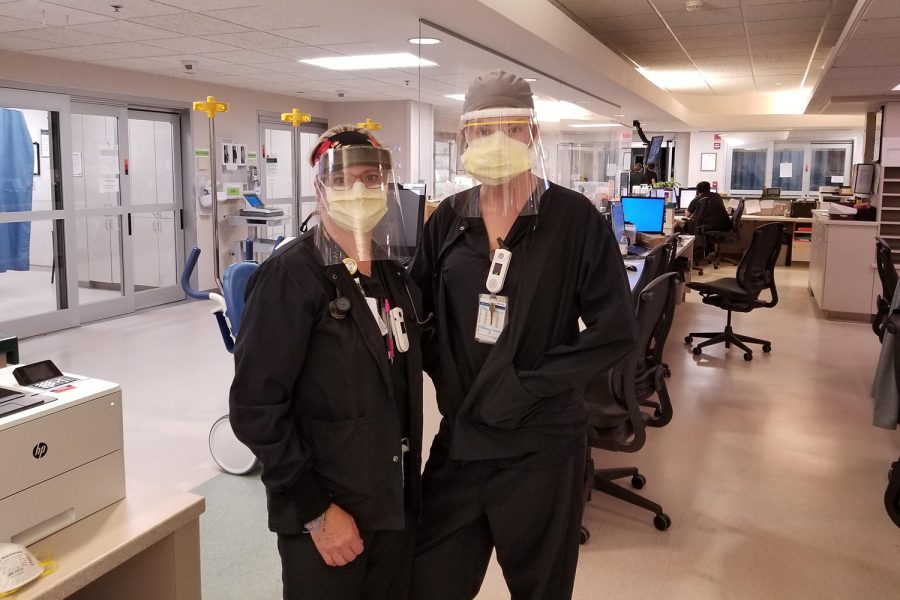
Morgan said in-patient unit nurses have shifted their skill sets. They follow social-distancing protocols, such as wearing masks and shields, every time they visit a patient before reaching out to the families. The liaison method has a tremendous effect on both sides, she said.
“We see these nurses coming in to work every day so happy,” Morgan said. “We are experiencing nurses creating relationships with these families, seeing how they are every day, and it also gives families the opportunity to ask questions. Clinical people are making the calls, and they know they have someone on the phone to help them navigate the information.”
Nurse Manager Penny Yenter, who oversees the COVID-19 unit at Mercy Iowa, said nurses work between eight- and 12-hour shifts to ensure the same nurse can stay with the same patient to build trust between them, the patient, and their family.
“It is nursing 101,” Yenter said. “We have always been available to families. The world we live in, we don’t always have families in our areas. That communication with family members for us [at Mercy] has always been important.”
She said COVID-19 disrupted the connection that traditionally develops between patients and nurses. Patients cannot see the smiling faces of their nurses — only their eyes — because everything else is covered to prevent COVID-19 spread, she said.
“When patients have been discharged or found to be negative,” Yenter said, “… they will say to us, ‘Wow, I get to see your face finally. It’s so nice.’”
Yenter said the IT Mercy team was critical in providing the necessary technology to continue fostering connections between patients, families, and the hospital. She said the team checked WiFi signals and phone connectivity in each room and set up iPads and Samsung tablets to make communication within the hospital as easy as possible.
Setting up the technology went smoothly, Yenter said, but helping patients utilize the equipment was more difficult than anticipated.
“For people my age and younger, [technology] is something run of the mill,” Yenter said. “COVID-19 affects the older generation greatly, especially those in care facilities. They may not use technology on a daily basis, so it is more of a struggle for them.”
After making technology easily accessible, Yenter said it was a joy to see patients interacting with families through Zoom, text messages, and other virtual forms of communication.
“A family sent a gentleman patient a video of him singing gospel songs with his daughter,” Yenter said. “It was like she was in the room. His face lit up, and it was beautiful. [Nurses] help with the physical, but the spiritual and emotional — that is just as important.”
Mercy Iowa City and UIHC both use phone calls as a primary communication tool, and Yenter said that communicating via phone instead of email allows families to hear the nurses’ voices.
“You can tell a lot from the sound of a person’s voice,” she said. “You can hear kindness, caring, and compassion, and that does not come across in an email.”
Yenter said Mercy Hospital is prepared to continue the nurse-liaison program and provide the same amount of support to patients affected and those who are not if the COVID-19 pandemic continues.
“We can all be in that family’s shoes, you know,” Yenter said. “We all know what it is like to not be able to see a loved one. We look for compassion when building our team, and if this lasts longer, I think we are ready for it.”