UI researcher identifies potential treatment for deadly pediatric cancer
The DEO of biochemistry at the University of Iowa was among a group of scientists who identified a class of drugs targeting cell metabolism that could lead to a new treatment for a prominent childhood cancer.
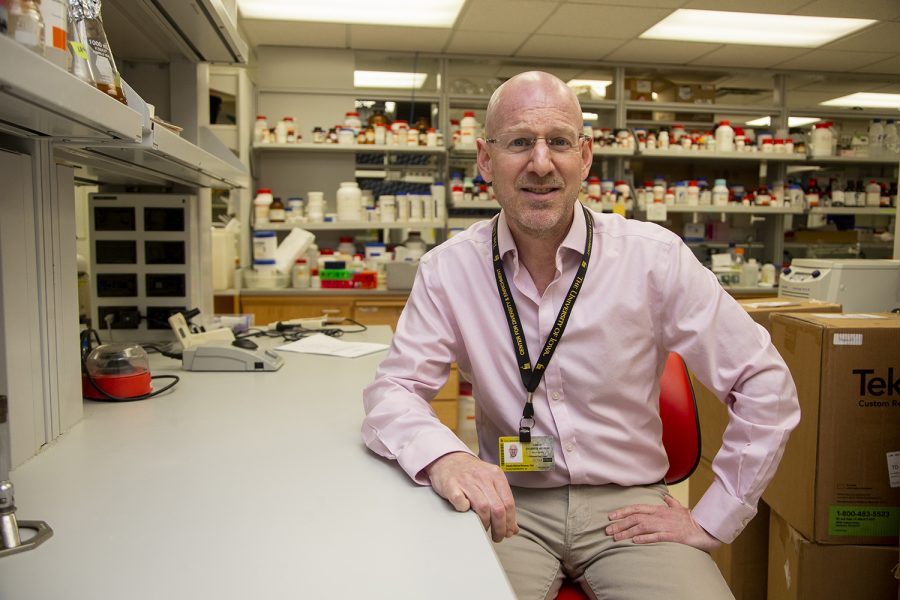
Dr. Charles Brenner, the DEO of biochemistry at the University of Iowa, poses for a portrait in his lab at the Bowen Science Building on Friday, August 30, 2019. Brenner is researching a class of drugs targeting cell metabolism that could lead to a new treatment for Diffuse Intrinsic Pontine Glioma, a rare and incurable childhood cancer.
September 3, 2019
After decades devoid of progress, University of Iowa professor and DEO of biochemistry Charles Brenner and a team of international researchers aim to provide a possible treatment for a deadly pediatric brain cancer.
In their initial report, the researchers focused on diffuse intrinsic pontine gliomas, or DIPG, an inoperable brainstem tumor found in children. The team concluded that a specific class of drugs have the potential to kill mutant tumor cells.
“The location of this tumor is ghastly,” Brenner said. “It frightens surgeons as much as it frightens parents, because you can’t safely get to it.”
According to the DIPG Resource Network, the median age of such patients is 6 to 7 years old with a median survival rate of less than a year. Progress on treatment has remained stagnant since the cancer’s discovery, senior author on the report and Translational Genomics Research Institute Deputy Director Michael Berens said.
Yale Cancer Center Associate Professor of Therapeutic Radiology Ranjit Bindra first discovered the mutation’s vulnerability to a metabolic inhibitor known as NAD a year into the study. Brenner was then contacted because of his discoveries involving NAD in the past, Bindra said.
“NAD is the central catalyst for metabolism,” Brenner said. “Metabolism is not only our ability to convert what we eat into energy, it’s our ability to convert everything we eat into literally everything we are.”
He added the NAD inhibitor is toxic to every cell, but particularly cells containing tumor mutations.
“We can use a tiny amount of a drug that inhibits NAD to eliminate those tumor cells at a level that normal cells can live with,” Brenner said.
He said researchers utilized a “therapeutic window” so that using a specific concentration is effective in eliminating the problem without becoming dangerous.
“The drugs that we’ve identified for these brain tumors are already being used in the clinic and have been tested in hundreds of patients,” Bindra added. “The drugs were shelved because they were too toxic or there was no clear indication to use them.”
Bindra said the team now has a biomarker to bring these drugs back into the mainstay of cancer treatment. Berens contributed greatly with his access to a library of pediatric brain tumor models with the specific mutation, Bindra said.
“[Translational Genomics Research Institute]’s involvement was primarily around the genomics and the patient-derived tumor models that we had available, to validate in human samples … that the mutation does cause vulnerability to treatment,” Berens said.
Bindra said the project became international once the team realized they needed additional pediatric brain tumor models that are rare in the scientific community, leading them to reach out to labs in the UK and Spain.
“Our work in this paper also demonstrates that other tumors would also be sensitive to this class of drugs,” said Bindra. “These mutations are also present in subsets of almost all cancers to varying degrees.”
Along with additional research, Brenner said the team is working on developing conditions for a clinical trial of the drugs with a small number of children to test response.
“My mom taught me that life is not always fair—this is an example where an innocent child is receiving a death sentence in his or her’s first decade,” Brenner said. “We want to be able to do something for these children.”