The Trump administration cuts cost-sharing reduction payments; while these cuts are controversial, they don’t affect Iowa’s proposed stopgap insurance plan.
By Isabella Senno
[email protected]
The federal government will end the Affordable Care Act’s cost-sharing reduction payments, which the Obama administration outlined to help low-income individuals get health insurance.
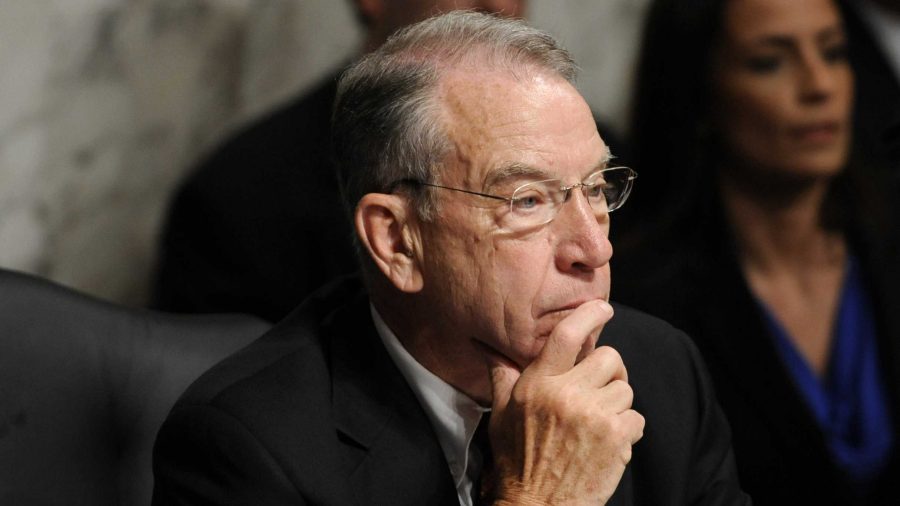
For Sen. Chuck Grassley, R-Iowa, these cuts have been a long time coming.
“Well-intended but poorly constructed incentives, including the Obamacare CSRs, foster a system of runaway spending,” Grassley said in an email to The Daily Iowan.
“President Trump has decided that he will follow the law and no longer fund these illegal subsidies.”
Iowa Attorney General Tom Miller joined nearly 20 other states on Oct. 13 in filing a lawsuit against the Trump administration. The suit argues that the federal government is not following a legal requirement to pay the subsidies and seeks to force continued payments.
Medica, a Minnetonka, Minnesota, insurance provider, is now the only option that remains open for consumers on Iowa’s individual insurance market for 2018. Geoff Bartsh, the vice president of individual and family business for Medica, said the company was well-prepared for the cuts and does not anticipate any major effect.
RELATED: Aetna, Wellmark roil health market
The insurer refiled its 2018 rates for individual health-insurance coverage with the Iowa Insurance Division in August, raising its premiums for silver-level plans by an average of 56.7 percent over 2017 rates.
“The decision by President Trump to end CSR payments will not change Medica consumer’s current health plans or change the options available to them in 2018,” Bartsh said in statement emailed to the DI. “This decision also has no impact on premium subsidies available to the vast majority of consumers. Our premiums for 2018 anticipated this action and were increased previously to account for it.”
The Iowa Insurance Division is based in Des Moines; it is also the agency that submitted the Iowa Stopgap Measure, a plan that, if approved by the federal government, would give Iowa the go-ahead to cut away at some of Obamacare’s key features.
Chance McElhaney, the communications director for the Iowa Insurance Division, said the Iowa measure was not affected by the Trump’s changes to the insurance subsidies.
“The final waiver submission for the Iowa Stopgap Measure only included Advanced Premium Tax Credit funds as a funding source, not CSR funds, so there is no impact on the Iowa Stopgap Measure,” he said in an email to the DI.
The proposed measure has gone through many procedures to get it to where it is now, including a federal comment period that ends today.
RELATED: Medicaid slices home for family
One commenter, identified as Nancy K. from Bellevue, Iowa, said she has felt the squeeze of high deductibles this year and will be forced to drop her insurance for 2018.
“Every single item, even our cemetery marker, is paid for or covered for my death in the event that we cannot afford insurance to pay for any so-called catastrophic health care,” she wrote.
If the stopgap measure is not approved in time, McElhaney said, up to 20,000 of the 72,000 Iowans in the market will be priced out.
“This is a federal problem, and we need a long-term solution from the federal government, or it needs to send the authority back to the states so that we can deal with the problems the ACA has created for Iowa’s individual health-insurance market,” McElhaney said.
Gov. Kim Reynolds, R-Iowa, said she has been attempting to reiterate the importance of speed to the Trump administration throughout the stopgap’s federal-approval process.
“We’re in touch with the White House almost every single day regarding the stopgap proposal,” she said. “The [Obamacare revision] waiver, it’s just not very flexible, they have us very boxed in, so we’re trying to be innovative and creative in a structure that is designed not to allow that, so it’s extremely frustrating to try to really find a solution so that Iowans have access to health care come Jan. 1.”