Some rural K-12 schools in Iowa look to telehealth access to provide health care for its students, but access to it is slim. University of Iowa researchers conducted a study to measure the causes and the effects of telehealth in schools.
The researchers found that 67.7 percent of rural students did not have access to a health care provider based on where they lived.
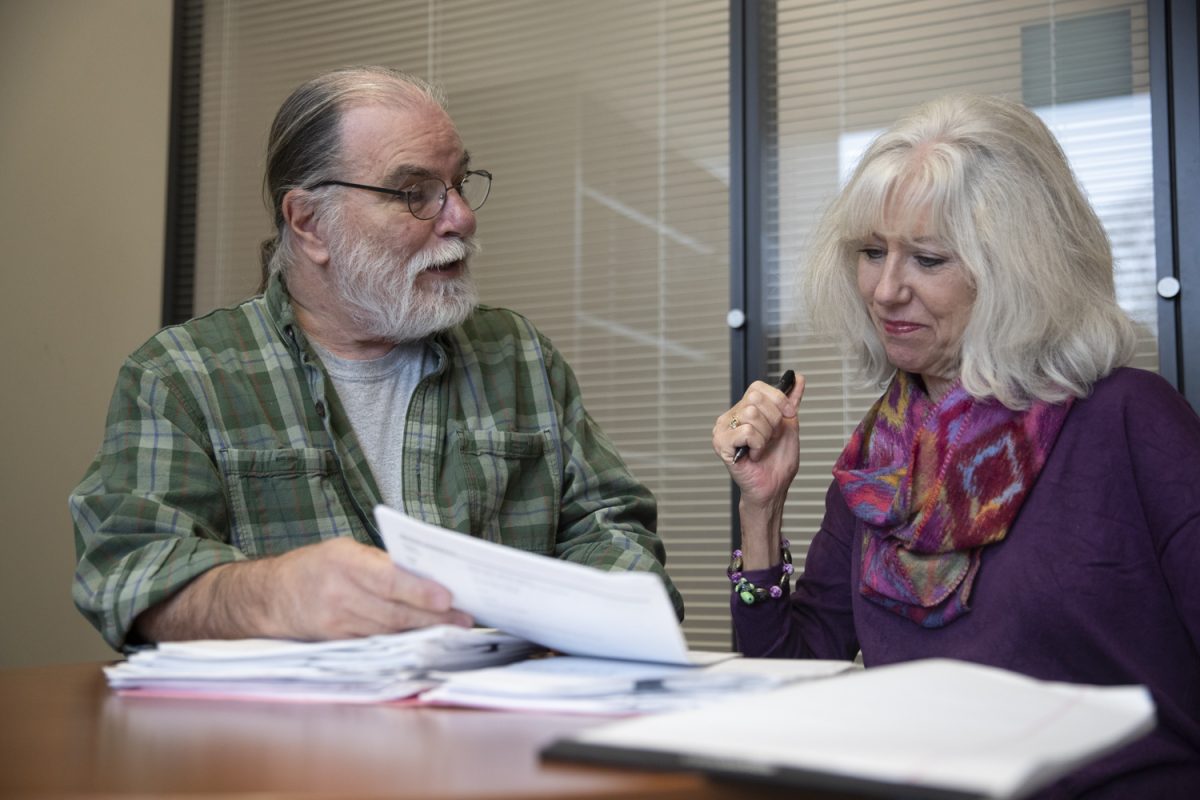
Marcia Ward, a distinguished professor at the UI College of Public Health, said the study started with grantees from across the country receiving funding from the Health Resources and Service Administration.
The study collected a variety of data, analyzing it, and writing about the findings in a series of papers.
Ward said the intention behind the study was to make people more aware of the problem and understand that in a rural area in particular, there is a shortage of providers.
“With these grantees, we had them focus specifically on particular shortages in underserved rural communities where they formed relationships with schools in their area,” Ward said.
A shortage of nurses in schools is one of the most significant findings from the study in urgent and primary care.
Though it would be ideal to have full-time nurses in each of these rural schools, Ward said it almost never happens, and telehealth provided a potential solution to that.
Instead of taking the student out of school or parents potentially missing work, Ward said telehealth allows children with relatively minor injuries to use the service.
“Lots of the negatives such as cost of appointment, travel, and others can be avoided by using telehealth and these services provided these students with nurses through a video call, even if the nurse is hundreds of miles away,” Ward said.
All appointments were made through telehealth with a registered nurse, or RN, and 95 percent of the time the problem was solved, preventing the student from having to leave school.
“That is the beauty of telehealth — it can be anywhere and can allow for quick access to needed clinicians,” Ward said.
Fred Ullrich, project director for research activities at the UI, said many students who had asthma, diabetes, oral health issues, and even behavioral health issues were able to be seen through this service and partially eliminate that lack of access to health care.
Ullrich said depending on which service a student required, a provider would be involved and offer the specific service needed. For example, telehealth students with behavioral health problems would be able to be prescribed the appropriate medication needed as well as general counseling.
Students with primary care or urgent care needs, Ullrich said, would be able to receive medication, care, and follow-up services if deemed necessary. Student-athletes who needed a sports physical could also receive these physicals via telehealth.
“Most of these rural areas are getting these services via telehealth where they didn’t exist otherwise,” Ullrich said.
Another aspect of telehealth that the researchers looked at was the number of encounters students had with this service. Students with chronic conditions tended to be seen more frequently than other students.
For behavioral and health services, students were typically seen between one and six sessions a semester. Ward said since the pandemic, this telehealth service in particular has seen the most increase.
“People see the efficacy of telehealth, and the popularity for it will continue to grow,” Ward said.