The Iowa Department of Public Health reported in February that the number of flu-related deaths in the state this season has reached 185, and influenza activity has fallen from “high” to “moderate.”
“Flu activity this year has doubled since the last couple of years,” Stephen Scheckel, the chief quality officer at Mercy Hospital said.
The report stated Iowa hospitalizations have slightly declined this week, remaining on a plateau.
This flu season was expected to be more severe than previous ones. However, the extent of its severity remained hazy until it was in full swing.
“Although [Mercy Hospital] was prepared for this outbreak, we didn’t know it would be this bad,” Scheckel said.
Despite this, hospitals were able to accommodate the increased number of patients.
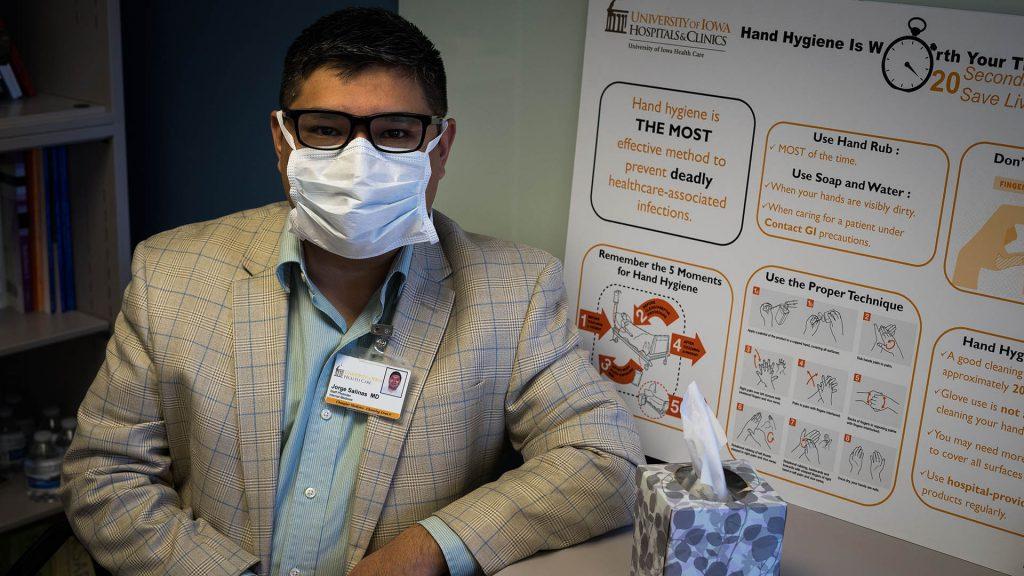
“[As] we prepared to see more cases, we maximized our coverage,” said Clinical Assistant Professor Jorge Salinas, an infectious disease specialist at the University of Iowa Hospitals & Clinics.
UIHC has a bio-emergency team that meets regularly to monitor influenza activity and ensure that enough supplies for treatment are stocked in order to tackle any surge, he said.
The UIHC suffered a shortage of surgical masks, which are used to prevent flu transmission from patients to workers at the time of the outbreak, Salinas said.
To contain the outbreak, communication campaigns were launched encouraging people to get vaccinated, Salinas noted. UIHC promoted the use of eCare and QuickCare, both of which allow people to be seen by a physician without going to the hospital.
UIHC also limited the number of visitors to two and recommended visitors to leave their children at home, he said.
“It is interesting because often what we see in the Southern Hemisphere can serve as a predictor as to how the flu season would be in the north,” Salinas said. “We used surveillance data from influenza activity in other countries to predict [how severely it would affect the U.S.].”
This strain of influenza, H1N3, originated in animals at some point and was then transmitted to humans, Salinas said.
Vaccines are readily available, but they are not always effective, Salinas said. Scheckel said this year’s vaccine was around 30 to 35 percent effective.
Mercy Hospital took an initiative to encourage its staff to get vaccinated and to wear masks to ensure they do not spread the flu.
“This way, we made sure we were a part of the solution, not the problem,” Scheckel said.
UI Student Health & Wellness saw a 70 percent increase in the number of students getting vaccines in January compared with last year. In February, there was a 40 percent increase over last year in the student-vaccine number.
“Students started coming in much later into the flu season to get their shots than previous years,” said Lisa James, the Student Health associate director for clinical outreach.
This shows students came in only after the flu was talked about and the scare was created, James said, and after parents prompted students to get vaccinated.
Physicians suggest there is still room for improvement when it comes to raising awareness about flu shots. Researchers are working on a universal vaccine that could contain flu outbreaks in the future, Scheckel said.
“We need to continue researching to find a better vaccine against influenza,” Salinas said.
A vaccine’s coverage of the flu, and the extent to which it matches, varies each year. Although the predictions can go wrong, vaccines must be produced ahead of time, Salinas said.